A global call for Universal Masking in the COVID-19 Pandemic
A Call for Action recommended by Dr. Bettina Horster, Chair Diplomatic Council Healthcare Forum, based on scientific research by De Kai PhD MBA, HKUST (University of Science & Technology), Hong Kong, International Computer Science Institute, Berkeley, CA, USA dekai cs [dot] ust [dot] hk dekai
cs [dot] ust [dot] hk dekai icsi [dot] berkeley [dot] edu @dekai123 http://dek.ai; Alexey Morgunov, University of Cambridge, UK, Manifold Research, Cambridge, UK asm63
icsi [dot] berkeley [dot] edu @dekai123 http://dek.ai; Alexey Morgunov, University of Cambridge, UK, Manifold Research, Cambridge, UK asm63 cam [dot] ac [dot] uk alexey
cam [dot] ac [dot] uk alexey manifoldresearch [dot] com @AlexeyMorgunov; Guy-Philippe Goldstein MBA, Ecole de Guerre Economique, Paris, France guyphilippeg
manifoldresearch [dot] com @AlexeyMorgunov; Guy-Philippe Goldstein MBA, Ecole de Guerre Economique, Paris, France guyphilippeg gmail [dot] com @guypgoldstein,Vishal Nangalia PhD MBCB FRCA, University College London, UK ELU AI Ltd, London, UK Royal Free Hospital, London, UK, vishal [dot] nangalia
gmail [dot] com @guypgoldstein,Vishal Nangalia PhD MBCB FRCA, University College London, UK ELU AI Ltd, London, UK Royal Free Hospital, London, UK, vishal [dot] nangalia gmail [dot] com @v_alien, Anna Rotkirch PhD, Population Research Institute, The Family Federation of Finland anna [dot] rotkirch
gmail [dot] com @v_alien, Anna Rotkirch PhD, Population Research Institute, The Family Federation of Finland anna [dot] rotkirch vaestoliitto [dot] fi @AnnaRotkirch, https://blogs.helsiki.fi/rotkirch.
vaestoliitto [dot] fi @AnnaRotkirch, https://blogs.helsiki.fi/rotkirch.
Please see here for scientific background.
As governments plan how to exit societal lockdowns, universal masking (mass face mask wearing) has rapidly emerged as one of the key non-pharmaceutical interventions for containing the spread of the COVID-19 pandemic. A growing body of evidence, ranging from clinical trials to the policy comparisons and new simulations presented here, suggests that universal masking as currently practiced in Asian countries significantly lowers rates of transmission.
Currently, the lowest recorded daily growth rates in COVID-19 infections are found in countries with a culture of mass face mask wearing, most of whom have also made mask wearing in public mandatory during the epidemic, and most of whom are not currently locked down. Supporting this correlational evidence, we provide a simulation of the effects of mass face mask wearing over time compared to effects of social distancing and lockdown. Simulation results indicate that without masking, lifting lockdown after nine weeks while keeping social distancing measures will risk a major second wave of the epidemic in 4-5 months’ time. However, if four out of five citizens would start wearing cloth masks in public before the lockdown is lifted, the number of new COVID-19 cases could decline enough to exit lockdown and still avoid a second wave. If only every second person starts wearing a mask, infection rates would also decline substantially, if not fully enough to prevent the second wave of the epidemic.
We also offer a new interactive simulation of agent-based models showing how masking works.
This white paper shows the need for mass masking as an alternative to a continued lockdown scenario. For this strategy to be most effective, the vast majority of the population needs to adopt mask wearing immediately. When a well—timed “mouth-and-nose lockdown” accompanies the current “full body lockdown”, we can lower both the human and economic costs of this pandemic.
With Europe, several US states, and other countries’ states having imposed strict measures of social distancing and restrictions on movement in March 2020, governments now seek a sustainable pathway back towards eased social restrictions and a functioning economy. Mass testing for infection and serological tests for immunity, combined with mass contact tracing, quarantine of infected individuals, and social distancing, are recommended by the WHO and have become widely acknowledged means of controlling the SARS-CoV-2 virus until a vaccine is available.
A growing body of evidence suggests that universal masking or face mask wearing is an additional essential tool in the COVID-19 mitigation toolkit. Masks indisputably protect individuals against airborne transmission of respiratory diseases. A recent Cochrane meta-analysis found that masking, handwashing, and using gowns and/or gloves can reduce the spread of respiratory viruses, although evidence for any individual one of these measure is still of low certainty.
Face masks work both ways
Face masks work both ways. They can protect an infected person from spreading the virus (transmission). And they can limit how much the non—infected individual is exposed to the virus (absorption). Surgical masks most efficaciously reduce the emission of influenza virus particles into the environment in respiratory droplets. Comparing different mask materials, medical masks have been found to be up to three times more effective in blocking transmission compared to homemade masks? Still, although masks vary greatly in their ability to protect, using any type of face mask (without an exploratory valve) can help decrease viral transmission.
Masks may be especially crucial for containing the COVID-19 pandemic, since many infections appear to come from people with no signs of illness. For instance, around 48% of COVID-19 transmissions were pre-symptomatic in Singapore and 62% in Tianjin, China.“ Furthermore, the SARS-CoV-2 virus is known to spread through airborne particles5 and quite possibly via aerosolized droplets as well.6’7»8’° It may linger in the air for at least 30 minutes and travel up to 4.5 meters, or larger than the “safe distance” imposed by social distancing rules in public — the insight which prompted Chinese health authorities to encourage masks in early March.”
Previous modelling studies indicate that masking can be an effective intervention strategy in reducing the spread of a pandemic.“ Crucially, a high rate of masking (80% or more) may be needed in a population to provide efficient protection from influenza.” This is why masking needs to be universal and not restricted to individuals who think they may be infected. Furthermore, universal masking can reduce stigmatisation of ethnic groups, risk groups or the sick and contribute to public solidarity.”
Cultural Convergence on Universal Masking
The Czech Republic was the first non-Asian country to embrace'and impose mandatory universalmasking on March 11. The Czech policy swiftly inspired various initiatives from citizens, journalists and scientists; and created global movements such as #masks4all and #wearafuckingm5sk. Their apguments build on the ability of the COVID-19 virus to spread from pre- and asympwmatic individuals who may not know that they are
Leading political and medical experts who early were advocated masking includecf Chinese {DC director-general Prof. George Fu Gas,‘ former FDA commissioner Scott Gottlieb and Prof. Caitlin Rivers & Johns Hopkins,” and the American Enterprise lnstitute’s Roadmap.‘ In early April a rapidly increasing number of governments of countries without a previous culture of mask wearing require or recommend universal masking including the Czech Republic, Austria and Slovakia. Additionally, public health bodies in the USA, France or New Zealand have moved toward universal masking recommendations.
The WHO has issued guidelines discouraging the use of masks in the public.” In early April the WHO modified the guidelines, allowing self-made masks but rightly stressing the need to reserve medical masks for healthcare workers.‘4»‘5 The policy shifts of the WHO and other CDCs reflect advances in our scientific understanding of this pandemic, and partly legitimize the altruistic “mask resistance” of civil society in this war against COVID-19.
The places that best handled COVID-19 all had universal masking
The universal masking movement has been triggered by the striking country comparison of COVID-19 cases. The majority of regions that have so far best managed their outbreaks are masking cultures and include Taiwan, South Korea, Singapore, and Hong Kong.
Indeed, most East Asian countries have a widespread culture of masking which has intensified during the COVID-19 outbreak. Masking in public is required in Taiwan, metropolitan areas in China such as Shanghai and Beijing (as well as Guangzhou, Shenzhen, Tianjin, Hangzhou, and Chengdu), Japan, South Korea, and other countries.
Based on detected cases from Jan 23 to Apr 10 for the top countries/regions per GDP per capita in Asia, Europe, and the Americas, starting once 30 cases have been detected. Percentage of reduction from peak growth rates is calculated as the average number of new cases Apr 6-10, divided by the average of the three peak numbers of new daily cases.
On the other hand, countries which have adopted mass testing, tracking and quarantining, but lack a universal masking culture, have not yet seen a clear reduction in COVID-19 transmission rates. Although these correlations may be due to underlying unobserved factors, they call for further enquiry into the effects of masking. A recent macro—level regression analysis by economists at Yale University, taking into account masking cultures and times of country COVID-19 policy responses, estimated that growth of COVID-19 rates only half that of mask wearing countries — the growth rate of confirmed cases is 18% in countries with no pre-existing mask norms and 10% in countries with such norms, while the growth rate of deaths is 21% in countries with no mask norms and 11% in countries with such norms. The authors note that such a 10% reduction in transmission probabilities could correspond to a per capita gain of $3,000-6,000 per each additional cloth mask (!), and that the economic benefits of each medical mask for healthcare personnel could be 300000 substantially larger.
Building on the insights above, we simulated the relative impact of masking compared to the two main other societal non-pharmaceutical interventions, lockdown and social distancing.
Our model suggests a clear impact of universal masking. Without masking, but even without continued social distancing in place, once the lockdown is lifted, the infection rate will increase and almost half of the population will become affected. This scenario would potentially lead to over a million deaths in a population the size of the UK. A continued lockdown does eventually result in bringing the disease under control after around 6 months. However, the economic and social costs of a “full body lockdown” will be enormous, which strongly supports finding an alternative solution. In our models, social distancing and masking at both 50% and 80% of the population — but no lockdown beyond the end of May — result in substantial reduction of infection, with 80% masking eventually eliminating the disease.
The simulation was fitted to the current timeline in many Western countries, with a lockdown imposed March the 24th (day 1) and planned to be lifted on May 31st. Universal masking is introduced in April. The simulation continues for 500 days from day 0, or around 17 months.
These modelling results support the need for mass masking as an alternative to continued lockdown scenario. For this strategy to be most effective, the vast majority of the population needs to adopt mask wearing immediately.
The exponential effect of masking can be counterintuitive. We have constructed a new interactive simulation model to demonstrate how masks can significantly reduce virus spread, even if they are nonmedical or homemade.To gain a more concrete feel for how masks impact the dynamics of virus spread, try the interactive visualization at http://dek.a /masks4all
Together with mass testing for infection and serological tests, tracking and quarantining diagnosed cases, and social distancing measures, universal masking shows us the way towards a sustainable way of life in the age of the coronavirus.
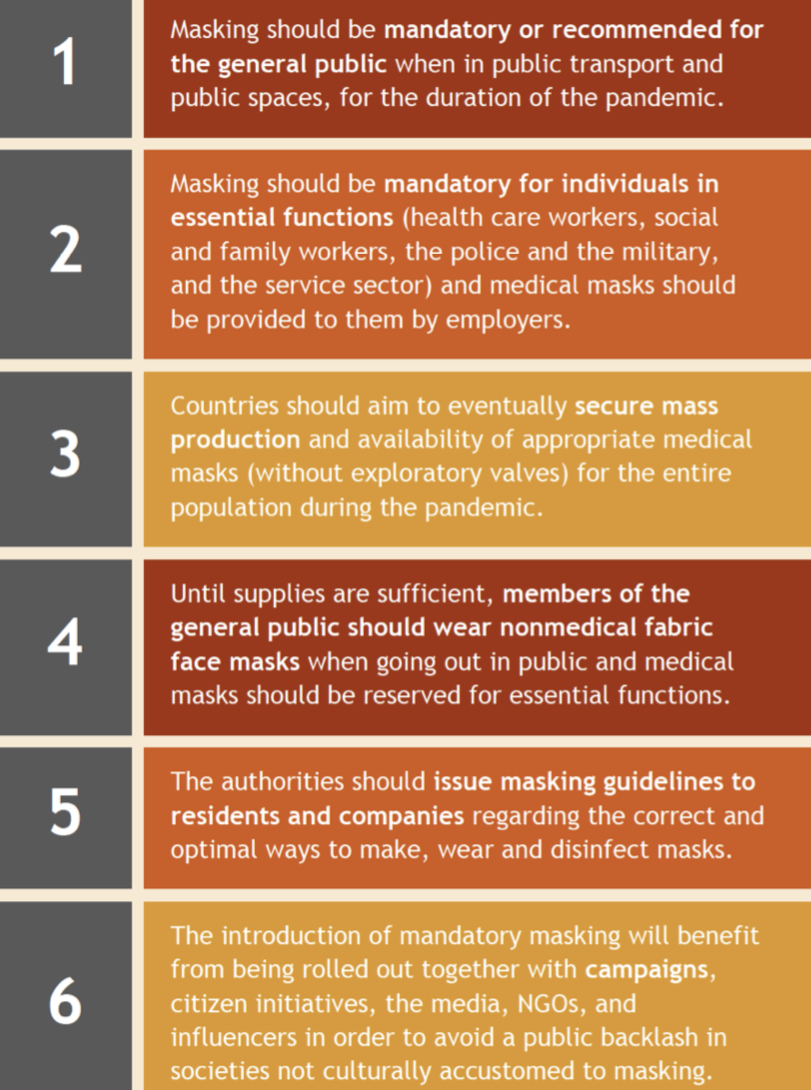
We urge Governments and international Bodies
We urge governments and international bodies who have not yet done so to consider masking as one of the key tools in population policy after the COVID-19 lockdowns and until the virus is under control. The analysis presented here supports recent studies,‘ suggesting that the effectiveness of universal masking is comparable to that of social distancing or a societal lockdown with closed workplaces, schools, and public spaces and limited geographical mobility. The results from our simulation help explain the dynamics behind the perplexing advantage in the Asian experience of tackling COV|D-compared to the situation elsewhere.
The effectiveness of universal masking in a given population is likely to depend on the type of masks used, the acceptance of masking in the population, the level of contagion of the virus, and what other interventions have been applied. From this perspective, the Central European experience will be highly informative, since it represents the first major shift to universal masking in a formerly non- masking culture. The effects of this pioneering intervention on infection rates and fatalities will appear only in the forthcoming weeks, although Slovakia and Slovenia are currently showing early indications of progress (see Figure 2 above). In any case, they illustrate that a country with no prior history of mask wearing in public may rapidly change course, and quickly adopt masks as a non-stigmatised — even street smart — way to express caring and solidarity in the community.
The medical and social risks of increased infections need to be countered by proper advice in the public domain. Some studies do indicate negative effects of cloth mass use, for instance, higher risks of infection due to moisture retention, reuse of cloth masks and poor filtration, in comparison to medical masks? There are also concerns that lay individuals may use both medical and/or cloth and paper masks incorrectly. Masking techniques and norms need to be taught with targeted information to different demographics, just as proper handwashing and social distancing techniques have been taught.